Introduction
Metabolic syndrome, or “Syndrome X,” as it is often called, is the combination of obesity, hypercholesterolemia, and hypertension linked by an underlying resistance to insulin. This condition is often associated with excess insulin secretion. The syndrome was first described by Reaven in 1998 (1), but its principal component of obesity was not initially emphasized. Retrospective data from the National Health Nutritional Survey for the period 1988 to 1994 implied that 47-million Americans had metabolic syndrome (2). The current prevalence of the syndrome may now be one in every four adults in the United States population, or about 70-million persons. So common and so pernicious are the negative health outcomes of metabolic syndrome that it qualifies as the number-one public health problem facing several Western societies.
Although the metabolic syndrome X is identified as a major cause of cardiovascular disease, it is less apparent that it increases deaths and disabilities from all causes, and underlies female reproductive disorders, polycystic ovary syndrome, non-alcoholic fatty-liver disease, non-alcoholic steatohepatitis, gestational diabetes mellitus, significant changes in body eicosanoid status, and certain cancers (3).
Rethinking the Management of Metabolic Syndrome
Excessive dietary intake of refined sugar, lack of exercise, poorly defined genetic tendencies, and adverse lifestyles contribute variably to the pathogenesis of the metabolic syndrome. Current pharmaceutical and surgical approaches to management of the syndrome have many disadvantages and limitations. It has been suggested that focused treatments of obesity, hypercholesterolemia, and hypertension that constitute the individual components of the syndrome are unlikely to provide a better outcome than are integrated management strategies (2). This suggestion is consistent with dietary attempts to restrict carbohydrate intake, and may explain the short-term success of some low carbohydrate diets for weight control (3). The notion of integrated management strategies opens the door for alternative management strategies with dietary supplements.
First-Line Management Options for Metabolic Syndrome
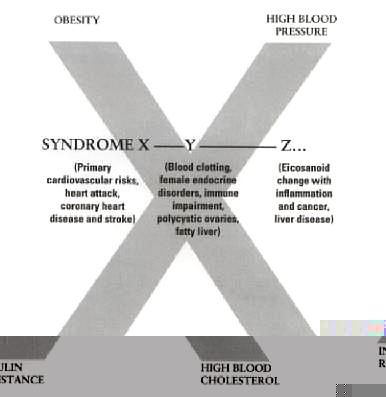
Metabolic syndrome has variable clinical manifestations, which I have attempted to incorporate in a new, unifying concept of disease. This concept extends beyond the existing definition of Syndrome X as obesity, hypertension and hypercholesterolemia linked by underlying insulin resistance. (3) In order to take account of this unifying concept, I have coined the term Syndrome X, Y and Z… to incorporate other diseases linked to insulin resistance (Figure 1). Effective prevention and treatment of metabolic syndrome involves a multifaceted approach directed at all of its cardinal components (3). Current allopathic treatments, which may have been too specifically focused on the individual components of metabolic syndrome, can be kept as a “back-up plan” for its management. In contrast, the natural techniques of lifestyle modification, and nutritional or nutraceutical interventions or both, may provide versatile and potent first-line options for its management (3). Table 1 presents a lifestyle-based program for managing the syndrome.
Figure 1: The concept of Syndrome X, Y and Z…, which includes the constellation of the hallmark components of Syndrome X (metabolic syndrome), to which are added other diseases, accounting for the Y and Z…component. The terms Syndrome X, Y and Z… are designed to emphasize the wide range of disabilities associated with the metabolic syndrome.
| Table 1. Lifestyle Program to Combat Metabolic Syndrome
Change in lifestyle, with specific avoidance of substance abuse, smoking cessation, and reduced intake of caffeine and simple sugars.
Behavior modification, including a change in eating patterns and amounts of various foodstuffs eaten. A modified low carbohydrate lifestyle with exclusion of simple sugar is valuable. Food that does not deliver a high glucose load is preferred (low glycemic index foods).
Exercise matched to the level of the subject’s aerobic fitness, with medical advice or advice from professional trainers, recommended before beginning an exercise program and periodically thereafter.
A diet with a reduced intake of simple sugars, salt, and saturated fat; a controlled protein intake; and an increased intake of healthy fats, such as essential fatty acids in fish oil.
Use of nutritional factors specifically designed for managing metabolic syndrome, including oat beta-glucan; antioxidants from berries; alpha-lipoic acid (ALA); chromium; biotin; vanadium; phaseolamin (Phase 2); vitamins that will reduce blood homocysteine levels.
|
The Effect of Dietary Fiber
Many types of soluble fiber may benefit individuals with metabolic syndrome, through their effects on appetite, body weight, and blood cholesterol levels (3). Evolution of research into soluble components of dietary fiber has led to the discovery of fractions of oat soluble fiber--beta-glucans--that have been shown to effectively lower blood cholesterol, reduce postprandial blood glucose, induce satiety, and suppress appetite (4-7). Although the glucocolloids that contain these beta-glucans have physicochemical properties that modulate upper gastrointestinal motility by delaying gastric emptying (8), and retard or impede the absorption of specific macronutrients in the form of glucose and fats, they also have intrinsic metabolic effects (IMEF). This IMEF occurs in part as a consequence of their fermentation in the colon to yield short-chain fatty acids, including propionic, acetoacetic, and butyric acids. Of these, propionic acid can enter the portal circulation of the liver, and may interfere with cholesterol synthesis by blocking the activity of hydroxymethyl-glutaryl coenzyme A (HMG CoA) reductase, a key enzyme in the synthetic pathway of cholesterol (4,6). Other types of soluble fiber are of value in blunting postprandial blood glucose responses, e.g. pectin and guar gum (10).
The Glycemic Index and the glycemic load of food are relevant to the dietary guidelines discussed above for counteracting metabolic syndrome (3,8). In simple terms, the Glycemic Index is a way of describing the ability of different foods to cause a rise in blood sugar. Foods laden with simple sugars can be expected to cause a rapid rise in blood glucose to high levels which, in turn, causes insulin secretion from the pancreas. Such foods have “High Glycemic Index.” A major component of the glycemic index is related to altered rates of sugar absorption. These are determined to a significant degree by altered rates of transfer of glucose to its site of maximal absorption in the small bowel, which is a function of the rate of gastric emptying (3,8,10). Speedy absorption of sugar pushes blood glucose levels high (a high glycemic response).
Essential Fatty Acids and Metabolic Syndrome
The influence of eicosanoids on glucose and insulin homeostasis has been defined partially (11), but the influence of insulin resistance (or lack) on eicosanoid pathways is less clear. Many individuals with Syndrome X have a dietary status where eicosanoid pathways are driven towards the production of prothrombotic and pro-inflammatory prostaglandins (3). This may occur largely as a consequence of dietary deficiency of certain essential fatty acids or alteration in the ratio of omega 6 and omega 3 essential fatty acid dietary intake. Furthermore, there is evidence that eicosanoid production can be modified by insulin lack and hyperglycemia. Animal studies show increases in a circulating metabolites of PGE2 production after the experimental induction of diabetes with streptozotocin (12). This rise in PGE2 metabolites is also found in diabetic humans (13). Thus, both the circumstances that contribute to the development of Syndrome X and insulin resistance within the metabolic Syndrome X can be expected to cause changes in the body eicosanoid status in a detrimental manner for health. This metabolic change in eicosanoid status is mainly a quantitative difference in the types of eicosanoid (prostaglandins) produced. More significant, it is known that among eicosanoid derivatives, eicosapentanoic acid (EPA) can enhance insulin sensitivity, presumably through effects on PPAR-receptors, which regulate the actions of insulin (3).
These observations open a path to the development of nutraceuticals and nutraceutical combinations tailored to specifically affect the function of the human genomic control of cell functions--or “genome-directed nutraceuticals.” In this context, some recent and highly popular diets for weight control require reappraisal (3). In particular, diets that provide a high saturated fat content with the goal of inducing dietary ketosis, such as the Atkins Diet, and diets involving protein-loading, such as the “Zone” Diet--both of which fall within the realm of low-carbohydrate diets--fail to provide some of the fats and fatty acids that appear to effectively combat metabolic syndrome. Specifically, diets intended to combat the syndrome should have more liberal contents of omega-3 and omega-6 fatty acids, in the correct balance with one another, together with a strictly controlled intake of refined carbohydrates, a restricted salt intake, an intake of fiber intake, and an increased proportion of vegetable sources of protein (9). Low carbohydrate diets that are proposed currently require facilitation to make them more effective in the long term and more healthy in terms of the global initiative of healthy weight control, with lowering of cholesterol blood pressure and combat against insulin resistance.
Table 2 presents a number of dietary components and supplements (3) that can help in preventing and managing metabolic syndrome.
| Table 2. Elements of Syndrome X (Metabolic Syndrome) and Nutritional Factors That May Counteract Them
Insulin resistance—Beta – glucan fractions of oat soluble fiber (Natures Benefit, Inc. Newark, NJ, USDA, US patent 6,060,519) may lower blood glucose levels after sugar intake. Chromium picolinate and polynicotinate (Nutrition 21, Inc., White Plains, New York) and alpha lipoic may assist insulin function.
Abnormal blood lipids--Oat beta-glucan may reduce blood levels of low-density lipoprotein (LDL) cholesterol, and triglycerides, and may variably increase high-density lipoprotein (HDL) cholesterol. Antioxidants and chromium with biotin may exert favorable effects on blood cholesterol.
Obesity--Oat beta-glucan may produce a sensation of satiety when taken before meals, and thereby assist in controlling calorie intake. Starch-blockers, such as Phaseolamin 2250 (Pharmachem, Hackensack, NJ) (Phase 2) may inhibit sugar absorption. Delayed appetite suppressant effects of fiber occur and smoothing out blood glucose responses may help to stop “sugar craving.”
Hypertension--Variable but small reductions in blood pressure result from weight control and lifestyle changes, e.g. exercise, avoidance of substance abuse (alcohol, caffeine and smoking), avoidance of supplements that allege metabolic enhancement, e.g. ephedra, and some ephedra alternatives. Soluble fiber may have modest independent blood pressure- lowering effects.
Oxidative stress and advanced glycation end products. This may be reduced by bioflavonoids, ellagic acid, anthocyanidins, alpha lipoic acid and other antioxidants.
Homocysteine--Vitamins B6, B12, and folic acid may reduce blood homocysteine levels.
|
Summary
Changes in lifestyle, and nutritional interventions with condition-specific dietary supplements (10), may have more to offer for the prevention and treatment of metabolic syndrome than do existing allopathic management strategies (3,10). Combating the specific components of this syndrome has become one of the most important public health initiatives in Western Society (3,10). In particular, the increasingly global initiative for achievement of a healthy body weight must be comprehensive in its tactics (3,10) and current low carbohydrate diets require modification and facilitation with revised dietary guidelines and the help of key dietary supplements or functional foods.
References
1. Reaven GM, Banting Lecture, 1988: Role of insulin resistance in human diabetes. Diabetes 37:1595,1998.
2. Ford ES, Giles WH, Dietz W. The prevalence of metabolic syndrome in the US population. JAMA 297(3):356-359, 2002.
3. Holt, S. Combat Syndrome X, Y and Z… Newark, NJ: Wellness Publishing, 2002.
4. Braaten JT, Wood PJ, Scott FW, et al. Oat beta-glucan reduces blood cholesterol concentration in hypercholesterolemic subjects. Eur J Clin Nutr 48:465-474.1994.
5. Inglett GE. Nutrient patent for beta glucan from cereals. U.S. Patent No. 6,060,519, 2000.
6. Glore SR, Van Treeck D, Knehans AW. Guild M: Soluble fiber and serum lipids. A literature review. J Am Diet Assoc 94:425-436, 1994.
7. Hallfrisch J, Schofield DJ, Behall KM. Diets containing soluble oat extracts improve glucose and insulin responses of moderately hypercholesterolemic men and women. Am J Clin Nutr 61:379-82, 1995.
8. Holt S, Heading CR, Carter D, et al. Effect of gel fiber on gastric emptying and absorption of glucose and paracetamol in humans. Lancet 1:636-639, 1979.
9. Holt S. The Soy Revolution. New York: Dell Publishing, Inc., 1999.
10. Holt S, Wright JV, Taylor TV. Syndrome X Nutritional Factors. Newark, NJ: Wellness Publishing, 2003 (in press)
11. Robertson RP. Eicosanoids as pluripotential modulators of pancreatic islet function. Diabetes 1988; 37:367
12. Axelrod L, Levine T. Plasma prostaglandin levels in rats with diabetes mellitus and diabetic ketoacidosis. Diabetes 1982; 31:994
13. McRae JR, Day RP, Metz SA, et al. Prostaglandin E2 metabolite levels during diabetic ketoacidosis. Diabetes 1985; 34:761
Also read: Natural Approaches To Diabetes Mellitus and Diabetes and Syndrome X